Have you ever felt trapped between two battles, fighting both mental health challenges and substance use at once? You’re not alone. Dual diagnosis affects over 21.5 million adults nationwide, and Colorado reports one of the highest rates in the country. This condition, where mental health disorders and substance use disorders occur together, creates a complex cycle that demands specialized care.
Coping with dual diagnosis requires more than willpower. It demands integrated strategies that address both conditions at once. When you treat one without the other, recovery often falls short. This guide provides practical, evidence-based approaches designed specifically for Colorado residents. You’ll discover local resources, daily management techniques, and professional support options in the Denver area.
Whether you’re starting your recovery journey or supporting someone who is, understanding how to navigate dual diagnosis makes all the difference. The path to wellness exists, and thousands have walked it successfully. Ready to take the first step? Call Revive Health Recovery at (303) 268-4655 for a confidential assessment.
Understanding dual diagnosis in Colorado’s context
What makes Colorado unique for dual diagnosis treatment
Colorado presents both challenges and opportunities for dual diagnosis treatment. The state ranks second nationally for mental illness prevalence, with 26.2% of residents experiencing poor mental health. High altitude, seasonal changes, and outdoor culture all influence mental wellness here. Denver’s urban environment contrasts with rural mountain communities, creating diverse treatment needs across the state.

The good news? Colorado has responded with robust behavioral health infrastructure. The Colorado Behavioral Health Administration oversees integrated care initiatives statewide. Denver houses extensive treatment networks, making specialized dual diagnosis care more accessible than in many states. Mountain communities offer unique therapeutic environments that support recovery through nature-based healing.
Access to medication-assisted treatment (MAT) has expanded significantly. Colorado providers now integrate MAT with mental health services, addressing both conditions simultaneously. This integrated approach aligns with current research showing that treating conditions separately leads to poor outcomes.
Struggling to find the right treatment approach? Contact Revive Health Recovery at contact@revivehealthrecovery.com to discuss personalized options.
Local statistics and prevalence rates
Understanding the scope of dual diagnosis in Colorado helps frame the importance of specialized care. Recent data reveals concerning trends. Colorado youth report the highest rate of major depressive episodes nationally. Adult substance use rates exceed national averages, particularly for alcohol and cannabis.
The bidirectional relationship between mental health and addiction creates unique challenges. Research shows shared neurobiological pathways involving dopamine and serotonin systems. When one condition worsens, it often triggers the other, creating a cyclical pattern that requires simultaneous treatment.
Gender differences emerge in Colorado’s dual diagnosis population. Women with co-occurring disorders more frequently report trauma histories. Men show higher rates of antisocial personality disorder alongside substance use. These patterns inform treatment planning at centers like Revive Health Recovery.
Relapse rates underscore the need for ongoing support. Approximately 50% of people with dual diagnosis experience relapse within 12 weeks after intensive treatment. This statistic highlights why long-term outpatient care and support groups prove essential for sustained recovery.
Available resources in the Denver metro area
Denver offers comprehensive resources for dual diagnosis treatment. The Denver Department of Public Health coordinates services across the metro area. Multiple outpatient centers provide integrated care, combining mental health and addiction services under one roof.
Revive Health Recovery stands out among Denver’s treatment options. Located at 1427 S Federal Blvd, the center specializes in outpatient dual diagnosis care. Their team understands that recovery demands more than separate treatments for each condition. They offer evidence-based therapies including Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and trauma-informed care.
Community resources complement professional treatment. The National Alliance on Mental Illness (NAMI) Colorado provides education and support groups throughout the metro area. Dual Diagnosis Anonymous meetings occur regularly in Denver neighborhoods. Peer recovery specialists, many with lived experience, offer mentorship through various community programs.
Transportation can challenge recovery efforts. Denver’s public transit system connects major treatment facilities. Many providers, including Revive Health Recovery, work with clients to address transportation barriers. Telehealth options have expanded, making initial consultations and follow-up appointments more accessible.
Need help navigating Denver’s treatment options? Call (303) 268-4655 for guidance from specialists who understand your situation.
Evidence-based coping strategies for daily management
Cognitive behavioral techniques for dual diagnosis
Cognitive Behavioral Therapy forms the foundation of effective dual diagnosis coping. CBT helps you identify thought patterns that fuel both mental health symptoms and substance use. The technique works by challenging negative thoughts before they trigger harmful behaviors.
Start by tracking your thoughts throughout the day. Notice when negative thinking emerges. Write down the situation, your immediate thought, and how it made you feel. This practice creates awareness of patterns you might not recognize otherwise. Over time, you’ll spot recurring themes that need attention.
Challenge distorted thinking with evidence. When your mind tells you something negative, ask yourself: “What proof supports this thought?” Often, you’ll find the evidence doesn’t hold up. Replace distorted thoughts with balanced alternatives. Instead of “I’ll never recover,” try “Recovery takes time, and I’m making progress each day.”
Practice behavioral activation alongside cognitive work. Depression and substance use both decrease activity levels. Schedule pleasant activities daily, even when motivation feels low. Start small with a short walk or phone call to a friend. Action often precedes motivation in recovery.
Apply these techniques consistently. The brain needs repetition to form new pathways. Morning and evening check-ins work well. Review your thought patterns, challenge unhelpful thinking, and plan positive activities for the day ahead.

Mindfulness and stress reduction methods
Mindfulness offers powerful tools for managing dual diagnosis symptoms. This practice teaches you to observe thoughts and feelings without judgment. Rather than fighting uncomfortable experiences, you learn to acknowledge them and let them pass.
Begin with simple breathing exercises. Find a quiet space and focus on your breath for five minutes. When thoughts arise, notice them without engaging. Return attention to your breathing. This basic practice reduces stress hormones and calms the nervous system. Both mental health and addiction recovery benefit from this physiological reset.
Body scan meditation helps identify where stress lives in your physical form. Lie down and slowly direct attention through each body part. Notice tension without trying to change it. This awareness often leads to natural relaxation. Regular practice improves your ability to catch stress before it escalates.
Colorado’s natural environment supports mindfulness practice. The mountains, parks, and outdoor spaces provide ideal settings for walking meditation. Choose a familiar trail and focus on sensory experiences. Notice sounds, sights, and physical sensations as you move. This practice combines the stress reduction benefits of nature with mindfulness techniques.
Incorporate mindfulness into daily activities. Wash dishes with full attention to the warm water and soap bubbles. Eat one meal per day slowly, savoring each bite. These micro-practices build the muscle of present-moment awareness throughout your day.
Want to learn mindfulness techniques specific to your situation? Revive Health Recovery offers personalized instruction. Call (303) 268-4655 to schedule a session.
Building healthy daily routines
Structure provides stability when coping with dual diagnosis. Your brain craves predictability during recovery. Consistent routines reduce decision fatigue and create space for healing practices. Start by establishing wake and sleep times that don’t vary by more than 30 minutes, even on weekends.
Morning routines set the tone for your entire day. Include activities that support both mental health and sobriety. Keep the sequence simple and achievable. Success builds momentum. Plan meals at regular intervals throughout the day. Blood sugar fluctuations affect mood and cravings. Eating every three to four hours maintains stable energy.
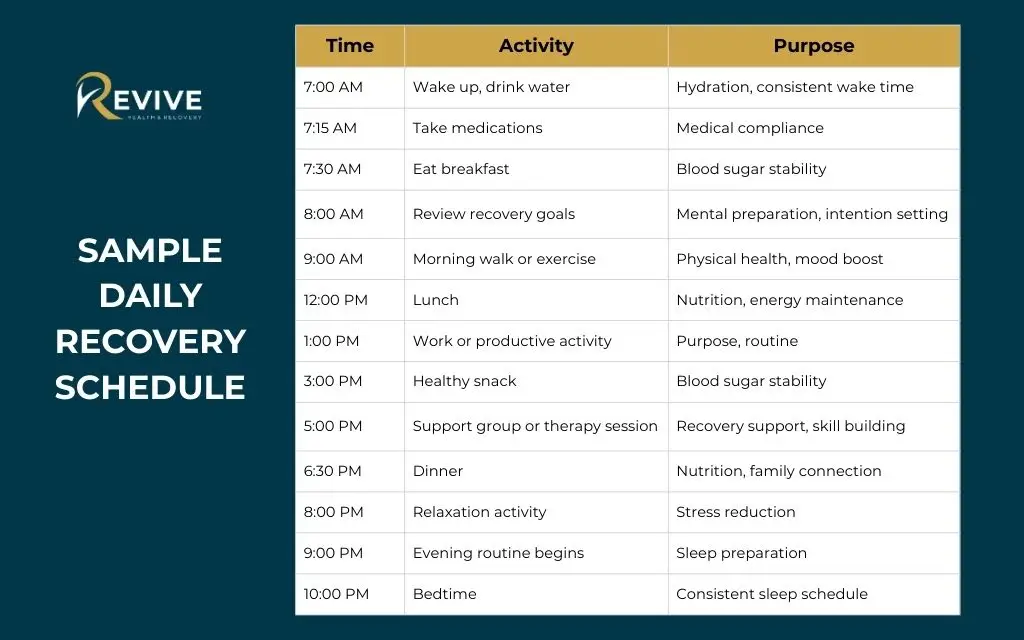
Sample Daily Recovery Schedule
| Time | Activity | Purpose |
| 7:00 AM | Wake up, drink water | Hydration, consistent wake time |
| 7:15 AM | Take medications | Medical compliance |
| 7:30 AM | Eat breakfast | Blood sugar stability |
| 8:00 AM | Review recovery goals | Mental preparation, intention setting |
| 9:00 AM | Morning walk or exercise | Physical health, mood boost |
| 12:00 PM | Lunch | Nutrition, energy maintenance |
| 1:00 PM | Work or productive activity | Purpose, routine |
| 3:00 PM | Healthy snack | Blood sugar stability |
| 5:00 PM | Support group or therapy session | Recovery support, skill building |
| 6:30 PM | Dinner | Nutrition, family connection |
| 8:00 PM | Relaxation activity | Stress reduction |
| 9:00 PM | Evening routine begins | Sleep preparation |
| 10:00 PM | Bedtime | Consistent sleep schedule |
Build recovery activities into your schedule like any other important appointment. Attend support groups at the same time each week. Schedule therapy sessions on consistent days. Exercise at a regular hour. These anchors create rhythm and accountability. They become non-negotiable parts of your day rather than optional extras.
Evening routines support quality sleep, which affects both mental health and recovery. Wind down one hour before bed. Dim lights, avoid screens, and practice relaxation techniques. Poor sleep disrupts the progress you make during the day. Protect your sleep schedule as fiercely as you protect your sobriety.
Medication management and medical compliance
Medications play a crucial role in many dual diagnosis treatment plans. Proper medication management requires attention and consistency. Missing doses or taking medications irregularly reduces their effectiveness and can trigger symptoms in both conditions.
Understand each medication’s purpose and how it supports your recovery. Ask your provider clear questions about timing, interactions, and expected effects. Write down instructions rather than relying on memory. Many people find it helpful to know why they take each medication. This knowledge increases commitment to the treatment plan.
Medication Safety Essentials Checklist
Daily Medication Routine:
- Use a pill organizer to track weekly doses
- Set phone alarms for medication times
- Link medication-taking to established habits (brushing teeth, eating meals)
- Keep medications in a visible, consistent location
- Maintain a current medication list in your wallet
Communication with Providers:
- Report all side effects, even minor ones
- Never stop medications without medical guidance
- Inform providers about over-the-counter medications and supplements
- Ask questions when instructions are unclear
- Request written instructions for complex regimens
Refill Management:
- Request refills one week before running out
- Keep pharmacy contact information accessible
- Use automatic refill programs when available
- Address insurance issues promptly
- Maintain backup supply for emergencies
Special Considerations:
- Store medications properly (temperature, moisture)
- Dispose of expired medications safely
- Never share medications with others
- Keep medications away from children and pets
- Bring medications to all medical appointments
Medication-Assisted Treatment (MAT) deserves special attention for substance use disorders. Medications like buprenorphine or naltrexone reduce cravings and support sobriety. When combined with mental health medications and therapy, MAT significantly improves outcomes for dual diagnosis.
Questions about your medication plan? Revive Health Recovery’s medical team can review your current treatment and suggest adjustments. Email contact@revivehealthrecovery.com for a consultation.
Building your support network in Colorado
Finding dual diagnosis support groups in Denver
Support groups provide connection with others who understand your experience. Dual Diagnosis Anonymous meetings occur throughout Denver, offering peer support specifically for co-occurring disorders. These groups follow a 12-step model adapted for the unique challenges of managing both conditions simultaneously.
The format varies by meeting. Some focus on sharing personal experiences. Others follow structured topics related to dual recovery. New members often feel anxious about first meetings. Remember that everyone there has faced similar struggles. The groups operate with confidentiality and respect. You only share what feels comfortable.
NAMI Colorado hosts support groups specifically for people managing mental illness and substance use. Their meetings occur at various Denver locations. Family members can attend separate groups designed for loved ones. This parallel support helps everyone in the recovery circle learn and grow together.
Online support options have expanded significantly. Virtual meetings eliminate transportation barriers and scheduling conflicts. Many people attend both in-person and online groups. This flexibility helps maintain connection during challenging periods when leaving home feels difficult.
Track which groups feel most helpful. Not every meeting will resonate with you. Try several different groups before deciding which to attend regularly. Some people find value in attending multiple groups throughout the week. Others prefer one consistent meeting. Your needs may change over time as your recovery progresses.
Need help finding the right support group? Call Revive Health Recovery at (303) 268-4655 for current meeting lists and recommendations.
Family and friends: creating a recovery circle
Recovery rarely succeeds in isolation. Your family and friends form a crucial support system when coping with dual diagnosis. However, loved ones often need education about co-occurring disorders to provide effective support. Help them understand that dual diagnosis requires treating both conditions together. Recovery doesn’t follow a straight line.
Set clear boundaries and expectations with your support network. Let loved ones know how they can help during difficult moments. Some people want phone check-ins. Others prefer space with occasional messages of encouragement. Communicate what works for you rather than expecting others to guess.
Family therapy strengthens recovery outcomes. These sessions help everyone understand how mental health and addiction affect relationships. Families learn communication skills and ways to support recovery without enabling. Many treatment centers, including Revive Health Recovery, offer family services as part of comprehensive care.
Create a crisis contact list with trusted individuals. Include people who can provide different types of support. One friend might excel at listening without judgment. Another might help with practical tasks during difficult periods. A family member might serve as your connection to professional help if symptoms escalate. Share this list with your treatment team.
Recognize that some relationships may not support your recovery. Establishing healthy boundaries sometimes means limiting contact with people who trigger symptoms or substance use. This decision can feel painful but proves necessary for your wellbeing. Your recovery circle should include people who respect your boundaries and support your goals.
Professional support team assembly
Your professional support team coordinates the multiple aspects of dual diagnosis treatment. In integrated treatment settings like Revive Health Recovery, these professionals work together rather than treating conditions separately.
Start with a comprehensive assessment to identify your specific needs. A thorough evaluation examines both mental health symptoms and substance use patterns. This assessment reveals how the conditions interact and influence each other. The results guide your treatment plan and determine which providers should join your team.
Your Recovery Team Roles
| Team Member | Primary Responsibilities | Meeting Frequency | Key Contributions |
| Primary Care Physician | Overall health monitoring, medical clearances, routine care | Every 3-6 months or as needed | Manages physical health conditions, coordinates with specialists, prescribes non-psychiatric medications |
| Mental Health Therapist | Individual counseling, skill development, emotional processing | Weekly or biweekly | Provides CBT, DBT, or trauma-informed therapy; helps develop coping strategies; processes difficult emotions |
| Psychiatrist | Medication management for mental health conditions | Monthly initially, then every 3 months | Prescribes and adjusts psychiatric medications, monitors side effects, evaluates medication effectiveness |
| Addiction Counselor | Substance use treatment, relapse prevention | Weekly in early recovery | Addresses addiction-specific issues, develops relapse prevention plans, teaches addiction coping skills |
| Case Manager | Practical support coordination | As needed, usually weekly check-ins | Assists with housing, employment, insurance, transportation; removes practical barriers to recovery |
| Peer Recovery Specialist | Mentorship from lived experience | Flexible, often weekly | Offers hope and practical advice from personal recovery experience, provides accountability |
| Prescriber for MAT | Medication-assisted treatment for addiction | Weekly to monthly depending on phase | Manages buprenorphine, naltrexone, or other MAT medications; monitors substance use |
| Family Liaison | Family education and support | Monthly or as requested | Educates family members, facilitates family therapy, improves family communication |
Peer recovery specialists bring lived experience to your support team. These individuals have successfully managed their own dual diagnosis recovery. They offer hope, practical advice, and understanding that comes from walking the same path. Their perspective complements professional expertise.
Ready to assemble your professional support team? Revive Health Recovery coordinates comprehensive care in one location. Call (303) 268-4655 to begin.
Peer recovery specialists and mentorship
Peer recovery specialists offer unique value in dual diagnosis treatment. These individuals have achieved sustained recovery from co-occurring disorders themselves. Their lived experience creates connection and hope that professional expertise alone cannot provide. They understand the specific challenges of managing mental health and addiction simultaneously.
Finding a peer mentor starts with treatment programs, support groups, or community organizations. Many outpatient centers, including Revive Health Recovery, incorporate peer specialists into their care teams. These relationships often begin formally through structured programs and may evolve into lasting friendships.
Mentorship provides practical strategies that work in real-world situations. Peers share what helped them through early recovery challenges. They offer perspective on navigating family relationships, employment, and social situations while maintaining sobriety and mental wellness. This guidance feels more accessible than clinical advice because it comes from someone who has lived it.
Regular check-ins with a peer mentor create accountability without judgment. You can discuss struggles honestly with someone who won’t shame you for setbacks. This non-clinical relationship complements professional treatment. Your mentor celebrates victories and helps troubleshoot obstacles as they arise.
Consider becoming a peer specialist yourself as your recovery strengthens. Helping others reinforces your own recovery and provides purpose. Training programs exist throughout Colorado for individuals interested in this rewarding work. Your experience becomes a gift that supports others beginning their journey.
Crisis management and relapse prevention
Identifying personal triggers and warning signs
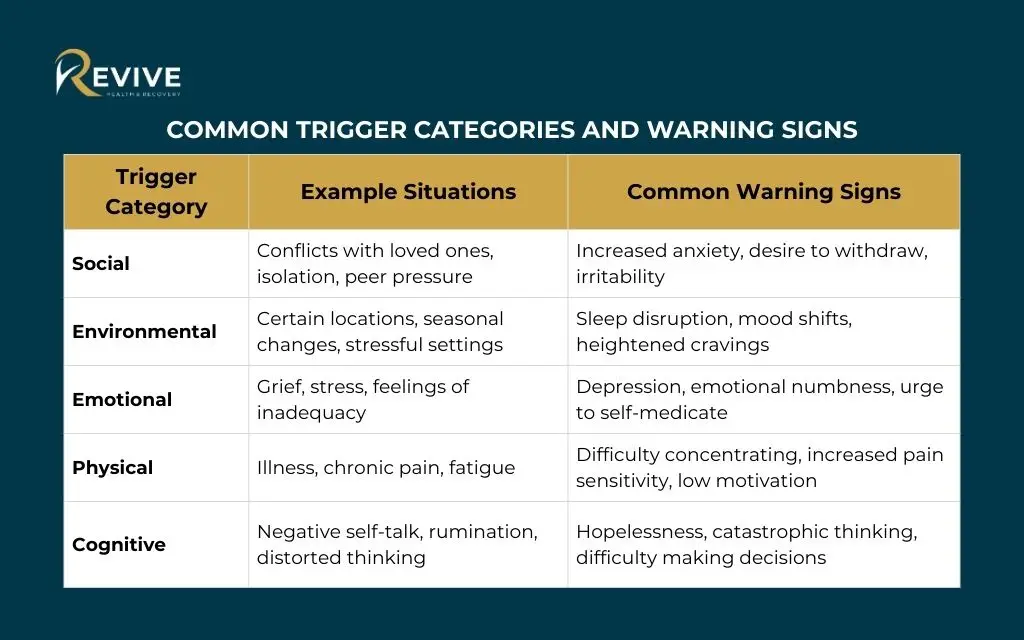
Understanding your personal triggers forms the foundation of effective crisis prevention. Triggers differ for everyone based on individual history, trauma, and life circumstances. Some triggers relate to specific places, people, or situations. Others involve internal states like hunger, anger, loneliness, or tiredness.
Create a detailed trigger inventory. Write down situations that have previously led to mental health symptoms or substance use. Include both obvious triggers and subtle ones. Perhaps arguments with family members precede depressive episodes. Maybe certain times of day trigger cravings. Financial stress might worsen anxiety. The more specific you become, the better you can plan ahead.
Recognize early warning signs before a full crisis develops. Your body and mind send signals when symptoms begin escalating. Common warning signs include sleep changes, appetite shifts, increased irritability, social withdrawal, and racing thoughts. Each person’s warning signs differ slightly. Track your patterns to identify your specific indicators.
Common Trigger Categories and Warning Signs
| Trigger Category | Example Situations | Common Warning Signs |
| Social | Conflicts with loved ones, isolation, peer pressure | Increased anxiety, desire to withdraw, irritability |
| Environmental | Certain locations, seasonal changes, stressful settings | Sleep disruption, mood shifts, heightened cravings |
| Emotional | Grief, stress, feelings of inadequacy | Depression, emotional numbness, urge to self-medicate |
| Physical | Illness, chronic pain, fatigue | Difficulty concentrating, increased pain sensitivity, low motivation |
| Cognitive | Negative self-talk, rumination, distorted thinking | Hopelessness, catastrophic thinking, difficulty making decisions |
Share your trigger list and warning signs with your support network. When you catch yourself early, others can too. Give permission for trusted individuals to point out warning signs they observe. Sometimes others notice changes before you do. This external perspective provides an additional safety layer.
Need help identifying your specific triggers? Schedule an assessment with Revive Health Recovery at (303) 268-4655.
Developing emergency action plans
Emergency action plans provide clear steps to follow during crisis moments. When symptoms escalate, decision-making becomes difficult. A pre-written plan eliminates guesswork and guides you toward safety. This document should exist in both physical and digital formats for easy access.
Outline specific steps to take when warning signs appear. Start with simple interventions you can do immediately. Perhaps you call your sponsor, practice breathing exercises, or remove yourself from triggering situations. Include backup steps if initial interventions don’t help. The final step should always involve reaching out for professional help.
Create separate sections for different crisis types. A panic attack requires different interventions than severe depression or substance use urges. Customize your plan to address the specific symptoms you experience. Include grounding techniques, distraction strategies, and people to contact for each situation.
Review and update your emergency plan regularly. Share copies with your treatment team and support network. Discuss the plan during therapy sessions to ensure it includes effective strategies. As you learn what works, refine the document. A living plan serves you better than something created once and forgotten.
Emergency Contact Quick Reference
| Resource | Contact Information | When to Use | Available Hours |
| Revive Health Recovery | (303) 268-4655 | Treatment questions, appointment scheduling, general support | 24/7 |
| Colorado Crisis Services Hotline | 1-844-493-8255 | Mental health crisis, substance use crisis, emotional distress | 24/7 |
| National Suicide Prevention Lifeline | 988 | Suicidal thoughts, self-harm urges, immediate danger to self | 24/7 |
| Text Crisis Line | Text HOME to 741741 | Text-based crisis support, prefer non-verbal communication | 24/7 |
| Your Primary Therapist | [Write name and number] | Mental health symptoms, therapy-related questions | [Write their hours] |
| Your Psychiatrist | [Write name and number] | Medication concerns, severe mental health symptoms | [Write their hours] |
| Your Sponsor/Peer Mentor | [Write name and number] | Substance use cravings, peer support, accountability | [Discuss their availability] |
| Trusted Family Member | [Write name and number] | Emotional support, practical help, safety monitoring | [Discuss their availability] |
| 911 or Local Emergency | 911 | Medical emergency, danger to self or others, severe withdrawal | 24/7 |
| Walk-In Crisis Center | [Find your nearest location] | Face-to-face crisis support, assessment, stabilization | Varies by location |
| Mobile Crisis Response | [Write local number] | On-site crisis assessment when you cannot travel | 24/7 in most areas |
Colorado crisis resources and hotlines
Colorado maintains extensive crisis resources available 24 hours a day. Colorado Crisis Services operates the state’s crisis hotline at 1-844-493-8255. Trained counselors provide immediate support, assess safety, and connect you with appropriate resources. Text and online chat options serve those who prefer non-verbal communication.
Walk-in crisis centers exist throughout the Denver metro area. These facilities offer immediate assessment and stabilization services without an appointment. Staff members evaluate your situation and determine the appropriate level of care. Services remain free regardless of insurance status or ability to pay.
Mobile crisis response teams come to you during emergencies. When someone cannot safely travel to a crisis center, these teams provide on-site assessment and intervention. They work to resolve crises in the least restrictive environment possible. Mobile teams understand dual diagnosis complexities and can coordinate with your existing treatment providers.
The Denver Department of Public Health operates specialized services for specific populations. Veterans, LGBTQ+ individuals, and Spanish speakers can access targeted crisis support. These specialized services acknowledge that different communities face unique challenges and may feel more comfortable with culturally competent care.
Emergency departments remain available when immediate medical attention becomes necessary. However, crisis hotlines and walk-in centers often provide more appropriate support for mental health and substance use crises. These specialized services offer therapeutic environments rather than medical settings. Staff training focuses specifically on behavioral health emergencies.
Experiencing a crisis? Call Colorado Crisis Services immediately at 1-844-493-8255. For ongoing crisis prevention support, contact Revive Health Recovery at (303) 268-4655.
When to seek immediate professional help
Recognizing when to seek immediate professional help can save your life. Certain symptoms require urgent intervention regardless of where you are in recovery. Never hesitate to reach out during these situations. Waiting can lead to dangerous outcomes.
Seek immediate help for any suicidal thoughts or self-harm urges. These symptoms signal a psychiatric emergency requiring professional assessment. Call 988 (National Suicide Prevention Lifeline) or go to the nearest emergency department. Crisis counselors can help you stay safe until professional help arrives.
Severe substance withdrawal requires medical supervision. Alcohol and benzodiazepine withdrawal can cause life-threatening seizures. Other substances produce dangerous physical symptoms. Contact your doctor or go to an emergency room if you experience shaking, confusion, hallucinations, or rapid heartbeat during withdrawal.
Significant changes in mental health symptoms warrant urgent evaluation. New or worsening psychotic symptoms, extreme agitation, or inability to care for basic needs require immediate attention. These changes might indicate medication adjustments or additional support needs. Don’t wait for your next scheduled appointment.
Relapse after a period of sobriety deserves immediate professional response. The shame surrounding relapse often prevents people from seeking help. Remember that relapse can be part of the recovery process. Reaching out quickly limits the damage and gets you back on track. Your treatment team expects occasional setbacks and wants to support you through them.
Safety concerns for yourself or others require immediate action. If you feel unable to keep yourself safe or notice concerning behaviors toward others, emergency intervention becomes necessary. Police involvement may occur in some situations. Crisis teams work to handle these situations therapeutically when possible.
Integrated treatment approaches available in Colorado
Outpatient vs. intensive outpatient programs
Choosing between outpatient and intensive outpatient programs depends on your current needs and stability. Both approaches treat dual diagnosis effectively while allowing you to maintain daily responsibilities. Understanding the differences helps you select the right level of care.
Outpatient vs. Intensive Outpatient Programs Comparison
| Feature | Standard Outpatient | Intensive Outpatient (IOP) |
| Session Frequency | 1-3 times per week | 3-5 days per week |
| Hours Per Week | 2-6 hours total | 9-20 hours total |
| Session Duration | 45-90 minutes per session | 3-4 hours per session |
| Best For | Stable symptoms, strong support system, lower risk | Stepping down from inpatient, need more structure than standard outpatient, moderate to high risk |
| Living Situation | Live at home | Live at home |
| Daily Responsibilities | Can maintain full-time work/school | May need part-time work or temporary leave |
| Treatment Components | Individual therapy, medication management | Group therapy, individual therapy, psychiatric services, case management |
| Duration | Ongoing as needed, often months to years | Typically 6-12 weeks, then step down |
| Cost | Lower per week | Higher per week but more intensive |
| Insurance Coverage | Usually covered with copay | Covered when medically necessary |
| Flexibility | High scheduling flexibility | Less flexible due to program structure |
| Support Level | Moderate professional support | High professional support with daily contact |
| Peer Connection | Limited peer interaction | Significant peer bonding through daily groups |
Revive Health Recovery specializes in outpatient services designed specifically for dual diagnosis. Their programs integrate mental health and addiction treatment in one location. This eliminates the confusion of coordinating separate providers. The team creates personalized recovery plans that evolve as your needs change.
Not sure which treatment level fits your situation? Call Revive Health Recovery at (303) 268-4655 for a professional assessment and recommendation.
Individual therapy options (CBT, DBT, trauma-informed care)
Individual therapy provides personalized attention to your unique challenges. Several evidence-based approaches show strong effectiveness for dual diagnosis. The right therapy depends on your specific symptoms, history, and treatment goals. Many people benefit from combining different therapeutic approaches.
Cognitive Behavioral Therapy (CBT) helps you identify and change thought patterns that contribute to both mental health and substance use issues. CBT teaches practical skills you can apply immediately. Sessions focus on present challenges rather than extensive past exploration. Most people see improvements within 12 to 16 weeks of consistent CBT work.
Dialectical Behavior Therapy (DBT) originally developed for borderline personality disorder but proves effective for various dual diagnosis presentations. DBT emphasizes emotional regulation, distress tolerance, mindfulness, and interpersonal effectiveness. Skills training occurs alongside individual therapy. The approach works particularly well when emotional dysregulation drives both conditions.
Trauma-informed care recognizes that trauma often underlies both mental health and substance use disorders. This approach creates safety in the therapeutic relationship before processing traumatic experiences. Trauma-informed therapists understand that seemingly resistant behaviors often represent protective mechanisms. They adapt treatment to avoid retraumatization while supporting healing.
Motivational Interviewing (MI) strengthens commitment to change. This collaborative approach resolves ambivalence about recovery. Rather than confrontation, MI uses empathy and strategic questions to help you identify your own reasons for change. The technique proves especially valuable in early recovery when motivation fluctuates.
Your therapist should have specific training in dual diagnosis treatment. Treating mental health or addiction separately misses the complex interaction between conditions. Revive Health Recovery’s therapists specialize in integrated approaches that address both simultaneously.
Group therapy and therapeutic communities
Group therapy offers unique benefits for dual diagnosis recovery. Connecting with others facing similar challenges reduces isolation and shame. Groups provide opportunities to practice interpersonal skills in a safe environment. The collective wisdom of group members often surpasses what any individual could offer.
Process-oriented groups focus on interpersonal dynamics and emotional experiences. Members share current struggles and receive feedback from peers. The therapist facilitates discussion and points out patterns. These groups help you understand how your behaviors affect others. This awareness supports healthier relationships outside of treatment.
Skills-based groups teach specific techniques for managing symptoms. Curriculum might cover stress management, communication, emotion regulation, or relapse prevention. Members practice skills during sessions and report on homework assignments. This structured format provides concrete tools you can apply immediately.
Dual diagnosis specific groups acknowledge the unique challenges of co-occurring disorders. Rather than separate addiction and mental health groups, integrated groups address both simultaneously. Participants understand that discussing one condition without the other misses important connections. This shared understanding creates powerful bonds.
Therapeutic communities extend group therapy principles into broader living environments. Some residential programs use this model. The community itself becomes the treatment tool. Members support each other’s recovery while addressing problematic behaviors through group process. Though less common than other approaches, therapeutic communities show strong outcomes for severe dual diagnosis.
Interested in group therapy options? Revive Health Recovery offers several group formats tailored to different needs. Contact contact@revivehealthrecovery.com to learn about current groups.
Medication-assisted treatment (MAT) options
Medication-Assisted Treatment combines medications with counseling and behavioral therapies for substance use disorders. MAT has proven particularly effective for opioid and alcohol use disorders. When integrated with mental health treatment, MAT significantly improves dual diagnosis outcomes.
For opioid use disorder, buprenorphine reduces cravings and withdrawal without producing euphoria. Methadone serves a similar purpose through specialized programs. Naltrexone blocks opioid effects, preventing relapse if someone uses. These medications allow your brain to heal while you develop recovery skills. They do not simply replace one addiction with another as some people incorrectly believe.
Alcohol use disorder responds to several medication options. Naltrexone reduces alcohol cravings and blocks rewarding effects. Acamprosate helps maintain abstinence by normalizing brain chemistry. Disulfiram creates unpleasant reactions if someone drinks. Your provider determines which medication best suits your situation based on your specific needs and medical history.
MAT works best when combined with therapy and support services. Medication alone rarely produces lasting recovery. The medications create stability that allows you to engage fully in treatment. They reduce the overwhelming symptoms that often derail early recovery efforts. This combination addresses both the biological and psychological aspects of addiction.
Mental health medications remain important alongside MAT. Antidepressants, mood stabilizers, and antipsychotic medications treat co-occurring mental health conditions. Your psychiatrist carefully monitors medication interactions. Some combinations require dosage adjustments. Open communication with your prescriber ensures safe and effective treatment.
Stigma unfortunately still surrounds MAT. Some people or programs view these medications as cheating or not being truly sober. This outdated thinking prevents many from accessing effective treatment. Research consistently shows that MAT increases recovery success rates. If MAT could help your recovery, let evidence guide your decision rather than stigma.
Lifestyle modifications for long-term success
Nutrition and physical health in recovery
Nutrition plays a significant role in both mental health and addiction recovery. Substance use often depletes essential nutrients. Poor mental health affects appetite and food choices. Addressing nutritional needs supports brain healing and overall wellness. Small dietary changes create meaningful improvements in mood and energy.
Eat regular meals at consistent times throughout the day. Skipping meals causes blood sugar fluctuations that trigger mood swings and cravings. Include protein with each meal to stabilize energy. Complex carbohydrates provide sustained fuel rather than quick spikes. Healthy fats support brain function. Balance becomes more important than perfection.
Certain nutrients deserve special attention during recovery. B vitamins support nervous system healing. Omega-3 fatty acids reduce depression and anxiety. Amino acids serve as building blocks for neurotransmitters. While supplements can help, food sources provide better absorption. Talk with your treatment team before starting any supplement regimen.
Hydration affects mental clarity and physical wellbeing. Aim for eight glasses of water daily. Dehydration worsens anxiety and fatigue. Many people mistake thirst for hunger or interpret it as cravings. Keep water accessible throughout your day. Add fruit for flavor if plain water feels boring.
Avoid using caffeine and sugar to manage symptoms. These substances create temporary relief followed by crashes. The roller coaster affects mood stability and recovery. Gradually reduce intake rather than stopping abruptly. Many people notice significant mood improvements after cutting back on caffeine and processed sugar.
Need personalized nutrition guidance for your recovery? Revive Health Recovery can connect you with resources. Call (303) 268-4655 to discuss comprehensive wellness planning.
Exercise and outdoor activities in Colorado
Colorado’s natural environment provides exceptional opportunities for recovery support through physical activity. Exercise releases endorphins that improve mood naturally. Regular movement reduces anxiety, improves sleep, and builds confidence. You don’t need intense workouts to gain benefits. Gentle, consistent activity works better than sporadic intensity.
Start with walking, the most accessible exercise for most people. Denver offers numerous trails suitable for all fitness levels. Walking combines physical activity with nature exposure. Both elements independently support mental health. Together, they create powerful recovery support. Begin with 10 to 15 minutes daily and gradually increase as you build stamina.
Hiking provides more intensive exercise when you feel ready. Colorado’s trails range from easy strolls to challenging climbs. Choose difficulty levels that match your current fitness. Hiking with others combines social connection with physical activity. Many recovery groups organize regular outdoor excursions. These outings build community while supporting wellness.
Yoga offers physical and mental benefits specific to dual diagnosis recovery. The practice combines movement with breath work and mindfulness. Many studios in Denver offer classes specifically for people in recovery. Trauma-informed yoga instructors understand how to create safe environments for healing. Even gentle yoga provides significant stress reduction benefits.
Consider cycling as weather permits. Denver’s extensive bike paths make this accessible year-round in many areas. Cycling provides cardiovascular benefits while allowing you to cover more ground than walking. The rhythmic nature of pedaling has a meditative quality. Many people find that exercise-induced endorphins significantly reduce cravings.
Winter sports keep you active during Colorado’s snowy months. Snowshoeing, cross-country skiing, and skating require minimal expense compared to downhill skiing. These activities maintain fitness during seasons when outdoor exercise becomes more challenging. The cold exposure itself has mood-boosting properties. Year-round outdoor activity supports consistent wellness.
Creative and recreational therapy options
Creative therapies access healing pathways that talk therapy alone cannot reach. Art, music, drama, and writing allow expression of experiences that words fail to capture. These modalities particularly benefit people who struggle with traditional therapy or have trauma histories. Creative expression can reveal insights and release emotions in safe ways.
Art therapy uses visual creation as a therapeutic tool. You don’t need artistic talent to benefit. The process matters more than the product. Drawing, painting, collage, and sculpture provide non-verbal outlets. Many find that creating art during difficult moments prevents unhealthy coping. Art therapy groups combine creative expression with peer support.
Music therapy harnesses sound’s power to influence mood and nervous system functioning. Listening to music, creating playlists, playing instruments, or songwriting all provide therapeutic benefits. Music activates multiple brain regions simultaneously. This engagement can interrupt rumination and reduce distress. Denver offers numerous music therapy programs through treatment centers and community organizations.
Writing and journaling support self-awareness and emotional processing. Regular writing about recovery experiences helps identify patterns and track progress. Poetry allows abstract expression. Narrative writing helps make sense of experiences. Gratitude journaling shifts focus toward positive aspects of recovery. Expressive writing reduces stress and improves immune function.
Drama therapy and psychodrama involve role-playing and theatrical techniques. These approaches help you explore different perspectives and practice new behaviors. Psychodrama might recreate challenging situations in safe environments. This experiential learning often creates deeper change than intellectual discussion alone. The techniques work particularly well in group settings.
Recreation therapy uses leisure activities therapeutically. Rock climbing teaches problem-solving and builds confidence. Team sports develop social skills. Adventure-based counseling incorporates challenge courses and outdoor experiences. These activities create opportunities for success outside of treatment settings. Achievement in recreation transfers to other life areas.
Curious about creative therapy options? Revive Health Recovery incorporates multiple therapeutic approaches. Email contact@revivehealthrecovery.com to learn about current offerings.
Employment and educational support services
Employment and education play crucial roles in sustained recovery. Meaningful work provides structure, purpose, and financial stability. Education opens opportunities and builds confidence. However, navigating these areas while managing dual diagnosis creates unique challenges. Support services help you succeed without sacrificing recovery.
Colorado Division of Vocational Rehabilitation serves people whose disabilities affect employment. Dual diagnosis qualifies for services. Counselors assess your abilities and goals. They provide job training, placement assistance, and workplace accommodations. Services include resume development, interview preparation, and career counseling. These supports continue after job placement to ensure success.
Educational accommodations support academic success while managing mental health and recovery needs. Disability services offices at colleges and universities coordinate accommodations like extended test time, reduced course loads, and mental health absence policies. Register with disability services early in each semester. Documentation from your treatment team establishes eligibility.
Part-time work often suits early recovery better than full-time employment. Reduced schedules allow time for therapy, support groups, and self-care. Financial pressures make this challenging for some. Explore whether family support, savings, or public assistance can supplement part-time income temporarily. Rushing back to full-time work before you’re ready increases relapse risk.
Disclosure decisions regarding your dual diagnosis require careful consideration. Employment law protects against discrimination for documented disabilities. However, stigma persists. Weigh the benefits of accommodations against privacy concerns. Your treatment team can help you think through disclosure decisions. Some workplaces prove more supportive than others.
Volunteer work provides many employment benefits without financial pressure. Volunteering builds skills, creates routine, and develops references. Many people find that giving back supports their recovery. Animal shelters, food banks, and community organizations welcome volunteers. Start with commitments you can maintain consistently. Success builds confidence for paid employment.
Navigating insurance and financial resources
Colorado Medicaid and mental health coverage
Colorado Medicaid (Health First Colorado) provides comprehensive mental health and substance use coverage. Eligibility extends to many adults with dual diagnosis due to income limits and disability provisions. Coverage includes therapy, psychiatric services, medications, and intensive outpatient treatment. Understanding your benefits removes financial barriers to recovery.
Application for Medicaid occurs through Colorado PEAK (Program Eligibility and Application Kit). The online portal allows you to apply and check eligibility. Many community organizations offer application assistance. Case managers can help navigate the process. Application typically takes 30 to 45 days for processing. Emergency Medicaid covers immediate needs while applications process.
Medicaid covers most evidence-based dual diagnosis treatments. Services include individual therapy, group counseling, psychiatric appointments, and medication management. Intensive outpatient programs receive approval when medically necessary. Prior authorization requirements apply to some services. Your provider handles this paperwork with your consent.
Choose providers who accept Medicaid to avoid out-of-pocket costs. Revive Health Recovery works with various insurance plans including Medicaid. Verify coverage before beginning treatment. Understanding your specific plan’s requirements prevents surprise bills. Coverage details vary between managed care organizations administering Colorado Medicaid.
Transportation assistance exists for Medicaid beneficiaries. If you lack reliable transportation to medical appointments, Medicaid may arrange rides. Contact your managed care organization to request this service. Regular therapy and psychiatric appointments become more feasible when transportation barriers disappear.
Questions about whether your insurance covers treatment? Call Revive Health Recovery at (303) 268-4655 for a free insurance verification.
Sliding scale and low-cost treatment options
Financial limitations should never prevent access to dual diagnosis treatment. Multiple options exist for people without insurance or with high deductibles. Sliding scale fees adjust costs based on income. Community mental health centers prioritize accessibility regardless of ability to pay.
Community mental health centers throughout Colorado offer sliding scale services. These centers serve as safety net providers. Fees decrease based on household income and size. Some clients pay nothing. Others contribute what they reasonably can. Services include therapy, psychiatric care, and case management. Quality does not diminish with reduced fees.
Faith-based organizations sometimes provide free or low-cost counseling. Quality varies between providers. Verify that counselors have appropriate credentials and dual diagnosis training. Some religious organizations offer excellent professional services. Others provide peer support without clinical training. Both can be valuable but serve different purposes.
University training clinics offer reduced-cost services. Graduate students provide therapy under licensed supervision. This arrangement benefits both parties. Students gain experience while clients access quality care at lower costs. Sessions may last longer due to consultation with supervisors. Many people appreciate the extra attention.
Free support groups provide invaluable peer support without any cost. Dual Diagnosis Anonymous, SMART Recovery, and NAMI groups welcome everyone. Attendance requires no financial contribution. While groups don’t replace professional treatment, they supplement therapy effectively. Regular group participation significantly enhances recovery outcomes.
Payment plans allow you to spread treatment costs over time. Many providers work with clients on affordable monthly payments. Discuss financial concerns openly with potential treatment centers. Revive Health Recovery understands that financial stress hinders recovery. They work with clients to create manageable payment arrangements.
Employee assistance programs (EAPs)
Employee Assistance Programs offer underutilized resources for dual diagnosis support. Most employers provide EAPs as a benefit. These programs typically include free short-term counseling, assessment services, and referrals. Benefits extend to household members in many cases. Services remain confidential from employers.
EAP counseling usually covers three to eight sessions per issue per year. A master’s level counselor provides assessment and brief treatment. If longer-term care becomes necessary, the EAP counselor refers you to community providers. Some programs offer additional sessions for complex situations. Short-term EAP counseling can stabilize crisis situations or help determine appropriate treatment levels.
Assessment services help determine what level of care you need. EAP counselors conduct thorough evaluations of mental health and substance use symptoms. They consider your support system, current stressors, and safety concerns. This assessment informs treatment recommendations. Many people find that professional assessment clarifies confusing symptoms and validates their experiences.
Referrals through EAPs often include quality guarantees. The EAP maintains relationships with local providers known for competent care. This vetting process eliminates trial and error in finding good treatment. Some EAPs negotiate preferred rates with providers. You might receive discounts beyond standard insurance coverage.
Work-life resources extend beyond mental health services. EAPs typically include legal consultation, financial planning, childcare assistance, and elder care support. These services address practical stressors that affect recovery. Solving concrete problems reduces overall stress levels. Lower stress supports both mental health and sobriety.
Contact your human resources department to access EAP services. Most programs offer 24-hour phone lines. Call anonymously to discuss concerns and available services. The conversation helps you decide whether to use benefits. Remember that EAP use remains separate from your employment record. Confidentiality protections allow you to seek help without workplace consequences.
Grant programs and community funding
Grant programs and community funding provide additional financial support for dual diagnosis treatment. These resources change frequently as new grants fund and others expire. Staying informed about available programs increases your access to support. Case managers and community organizations track current opportunities.
The Colorado Crisis Services system operates through community funding. Services remain free regardless of insurance or income. Crisis hotlines, walk-in centers, and mobile response teams accept everyone. These services provide immediate support during emergencies. They can also connect you with ongoing treatment resources.
SAMHSA (Substance Abuse and Mental Health Services Administration) funds various treatment programs nationally. Some Colorado providers receive grants that allow them to offer reduced-cost services. These grants typically target specific populations like veterans, pregnant women, or justice-involved individuals. Ask potential providers whether grant-funded slots exist.
County governments sometimes fund mental health and addiction services. Denver and surrounding counties maintain programs for residents who fall through other coverage gaps. Requirements vary by county. Contact local behavioral health offices to learn about available programs. Wait lists may exist for popular services.
Nonprofit organizations occasionally offer treatment scholarships. These opportunities typically involve application processes. You might need to write an essay or provide financial documentation. Awards range from partial fee reduction to full coverage. Recovery advocacy organizations sometimes maintain lists of scholarship opportunities.
Community fundraising helps some individuals access needed treatment. Platforms like GoFundMe allow people to raise money from personal networks. While asking for help can feel uncomfortable, many people find that communities respond generously. Be honest about your needs and how treatment will change your life. Personal stories resonate more than generic requests.
Need help identifying financial resources for treatment? Call Revive Health Recovery at (303) 268-4655 to speak with a financial counselor who understands available options.
FAQs about coping with dual diagnosis
What is the difference between dual diagnosis and co-occurring disorders?
The terms “dual diagnosis” and “co-occurring disorders” mean the same thing. Both refer to having a mental health disorder and substance use disorder at the same time. Some professionals prefer “co-occurring disorders” because people may have more than two conditions. Colorado treatment providers use both terms interchangeably. What matters most is that you receive integrated care treating all conditions together. Revive Health Recovery specializes in this integrated approach, ensuring nothing gets overlooked in your treatment plan.
How do I know if I need dual diagnosis treatment versus separate treatments?
You need integrated dual diagnosis treatment when mental health and substance use disorders influence each other. Signs include using substances to manage mental health symptoms, experiencing mental health symptoms that worsen with substance use, or finding that treating one condition doesn’t improve overall functioning. Separate treatments often fail because they don’t address how conditions interact. A comprehensive assessment reveals whether integrated care makes sense for your situation. Call Revive Health Recovery at (303) 268-4655 for a professional evaluation that identifies your specific needs and recommends the most effective treatment approach.
Are there specialized dual diagnosis programs in Denver?
Yes, Denver offers several specialized dual diagnosis programs, with Revive Health Recovery standing out for comprehensive outpatient care. Located at 1427 S Federal Blvd, they provide integrated treatment combining mental health therapy, addiction counseling, medication management, and support services in one location. Their team understands the complex interaction between mental health and substance use disorders. Denver’s extensive treatment network includes other options as well. However, finding truly integrated care requires careful research. Contact Revive Health Recovery to discuss how their specialized approach differs from treating conditions separately.
What should I do if my loved one has dual diagnosis but refuses treatment?
Refusal of treatment challenges families deeply. Start by learning about dual diagnosis yourself through organizations like NAMI Colorado. Express concern without judgment or ultimatums. Offer to help them access assessment services. Sometimes people fear treatment more than they refuse help. Address specific concerns about what treatment involves. Family therapy can open dialogue even before your loved one commits to personal treatment. In crisis situations, Colorado’s involuntary commitment laws allow emergency intervention when someone poses immediate danger. Revive Health Recovery offers family consultations to help you navigate this difficult situation. Call (303) 268-4655 to discuss strategies specific to your circumstances.
How long does dual diagnosis treatment typically take in Colorado?
Dual diagnosis treatment varies significantly based on individual needs, severity, and progress. Initial intensive phases often last three to six months. However, recovery represents a long-term process requiring ongoing support. Many people transition through levels of care over time. You might start with intensive outpatient care then step down to regular outpatient therapy. Medication management continues as long as needed. Support group involvement often extends indefinitely. The relationship between mental health and substance use disorders means sustained attention prevents relapse. Revive Health Recovery creates personalized treatment plans that evolve with your progress. Contact them at contact@revivehealthrecovery.com to discuss realistic timelines for your specific situation and how they support long-term success.
Finding professional help at Revive Health Recovery
When coping with dual diagnosis feels overwhelming, professional support makes the difference between struggling alone and finding sustainable recovery. Revive Health Recovery specializes in the unique challenges of co-occurring mental health and substance use disorders. Their Denver location at 1427 S Federal Blvd provides accessible outpatient care designed specifically for dual diagnosis.
What sets Revive Health Recovery apart is their integrated treatment philosophy. Rather than bouncing between separate providers for mental health and addiction, you receive comprehensive care in one place. The team includes therapists, psychiatrists, and case managers who communicate regularly about your progress. This coordination ensures that nothing falls through the cracks. Everyone working with you understands your complete situation.
Evidence-based therapies form the foundation of their approach. Cognitive Behavioral Therapy helps you identify and change thought patterns driving both conditions. Dialectical Behavior Therapy teaches emotional regulation skills. Trauma-informed care addresses underlying experiences that contribute to symptoms. Motivational Interviewing strengthens your commitment to recovery. The team selects therapeutic approaches based on your specific needs rather than applying one-size-fits-all treatment.
Medication management receives careful attention when appropriate. Psychiatric services help determine whether medications could support your recovery. The psychiatrist coordinates with your therapists to monitor how medications affect your symptoms and therapy progress. Medication-Assisted Treatment options exist for substance use disorders. All prescribing decisions consider your complete mental health and substance use picture.
Family involvement strengthens recovery outcomes significantly. Revive Health Recovery offers family services through a dedicated liaison who stays involved throughout your treatment. Family members learn about dual diagnosis and develop skills to support your recovery effectively. This approach recognizes that healing happens within relationships. Everyone benefits when families understand co-occurring disorders.
Practical support helps you maintain recovery while managing daily life. Case management services address barriers like transportation, housing, and employment. Support groups connect you with others who understand dual diagnosis challenges. The team helps you build a complete support network extending beyond clinical appointments. They understand that recovery requires more than therapy hours.
The outpatient model allows you to maintain responsibilities while receiving intensive support. You continue living at home, working if able, and staying connected with your support system. Treatment schedules accommodate real-world demands rather than requiring you to put life on hold. This approach helps you practice recovery skills in actual environments where you’ll use them long-term.
Starting treatment requires only a phone call. The admissions team conducts a free confidential assessment to understand your situation. They verify insurance coverage and discuss financial options. If Revive Health Recovery fits your needs, they schedule intake appointments quickly. You don’t wait weeks to begin getting help. The team knows that motivation fluctuates. They make starting treatment as simple as possible.
Conclusion
Coping with dual diagnosis presents real challenges, but recovery is absolutely possible. Thousands of people successfully manage co-occurring mental health and substance use disorders. The strategies outlined in this guide provide a roadmap for your journey. From understanding your triggers to building support networks, each element contributes to sustainable wellness.
Colorado offers extensive resources supporting dual diagnosis recovery. Denver’s treatment infrastructure particularly provides access to specialized care. You don’t have to navigate this path alone. Professional help, peer support, and community resources combine to support your success. The key lies in taking that first step toward integrated treatment.
Your recovery matters. The life you want exists on the other side of asking for help. Mental health and substance use disorders are treatable conditions, not character flaws. With proper support, you can build the stable, meaningful life you deserve. Don’t let another day pass struggling alone.
Take action today. Call Revive Health Recovery at (303) 268-4655 for a confidential assessment. Our team is available 24/7 to answer questions and help you begin your recovery journey. You can also email contact@revivehealthrecovery.com or visit them at 1427 S Federal Blvd, Denver, CO 80219. Hope starts with one conversation. Make that call today.



