Have you tried every physical treatment available, only to find your pain persists? You’re not alone. Chronic pain affects over 50 million American adults, and research reveals something remarkable: mental health treatment can significantly reduce physical pain symptoms. This isn’t because your pain exists only in your mind. Your pain is real. However, pain involves complex interactions between your nervous system, brain, and emotions.
At Revive Health Recovery in Denver, we specialize in evidence-based mental health treatment for chronic pain, helping Colorado residents break free from cycles of suffering. Whether you face fibromyalgia, chronic back pain, arthritis, or unexplained persistent discomfort, understanding how psychological therapies like Cognitive Behavioral Therapy and Pain Reprocessing Therapy address pain opens powerful pathways to healing.
This article explains how mental health treatment works for chronic pain, what approaches prove most effective, and how you can access care that fits your life.
Understanding the link between mental health and chronic pain
What is chronic pain? More than just physical symptoms
Chronic pain persists beyond three months, continuing long after normal tissue healing completes. This type of pain affects approximately 20% of adults nationwide, creating challenges that extend far beyond physical discomfort.
Scientists now recognize three main pain types:
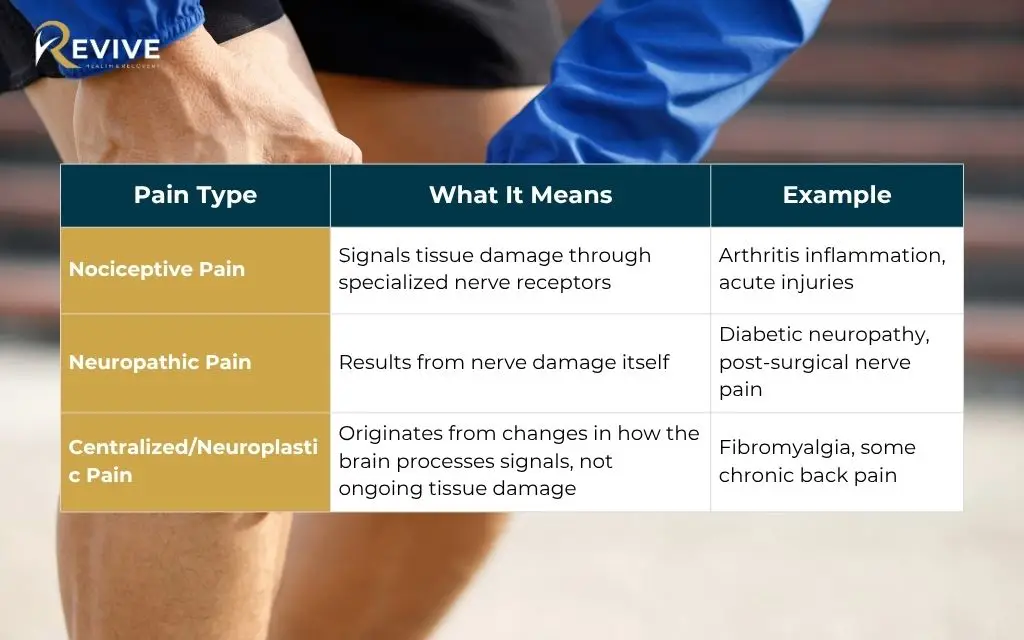
This third type represents a breakthrough in pain science. Your nervous system can develop heightened sensitivity, misinterpreting safe signals as dangerous. The brain creates pain even when no physical damage exists. This doesn’t make pain less real. Instead, it reveals why traditional physical treatments alone sometimes fall short.
Common conditions that respond to mental health treatment:
- Fibromyalgia and widespread pain syndromes
- Chronic lower back pain and neck pain
- Arthritis-related pain
- Neuropathic pain conditions
- Persistent headaches and migraines
- Complex regional pain syndrome
- Post-surgical chronic pain
- Medically unexplained pain symptoms
People living with chronic pain face four times higher rates of depression and anxiety compared to those without pain. The relationship works both ways. Pain affects mood, and mood influences pain perception.
The bidirectional relationship between pain and mental health
Chronic pain creates profound emotional challenges. Persistent discomfort disrupts sleep, limits activities you once enjoyed, and strains relationships. Many people describe feeling frustrated, isolated, or misunderstood.
Pain catastrophizing amplifies suffering through three mechanisms: rumination about pain, magnification of pain’s threat, and feelings of helplessness. Research using the Pain Catastrophizing Scale shows these thought patterns correlate with elevated inflammation markers and increased salivary cortisol levels.
The fear-avoidance cycle traps many in worsening disability. When movement causes pain, natural instinct suggests avoiding that movement. However, avoidance leads to physical deconditioning, making future movement more painful. The cycle continues, progressively limiting function.
Work performance suffers. Relationships become strained. Social connections fade. The emotional toll extends beyond the person experiencing pain, affecting entire families and support networks.
How mental health impacts pain perception
The biopsychosocial model recognizes that chronic pain results from biological, psychological, and social factors working together. This comprehensive framework explains why identical injuries produce vastly different pain experiences in different people.
Your brain processes all pain signals, meaning psychological factors inevitably influence pain intensity. Stress, anxiety, and depression don’t just accompany pain. These conditions amplify pain signals through measurable changes in brain activity.
Brain imaging studies demonstrate that psychological interventions actually change pain processing in regions like the anterior cingulate cortex. When you learn to manage thoughts and emotions related to pain, your brain responds by processing pain signals differently.
The mind-body connection operates continuously. Thoughts influence physical sensations. Physical sensations shape thoughts. This interconnection creates opportunities for healing through mental health treatment for chronic pain.
Evidence-based mental health treatments for chronic pain
Cognitive behavioral therapy for pain management
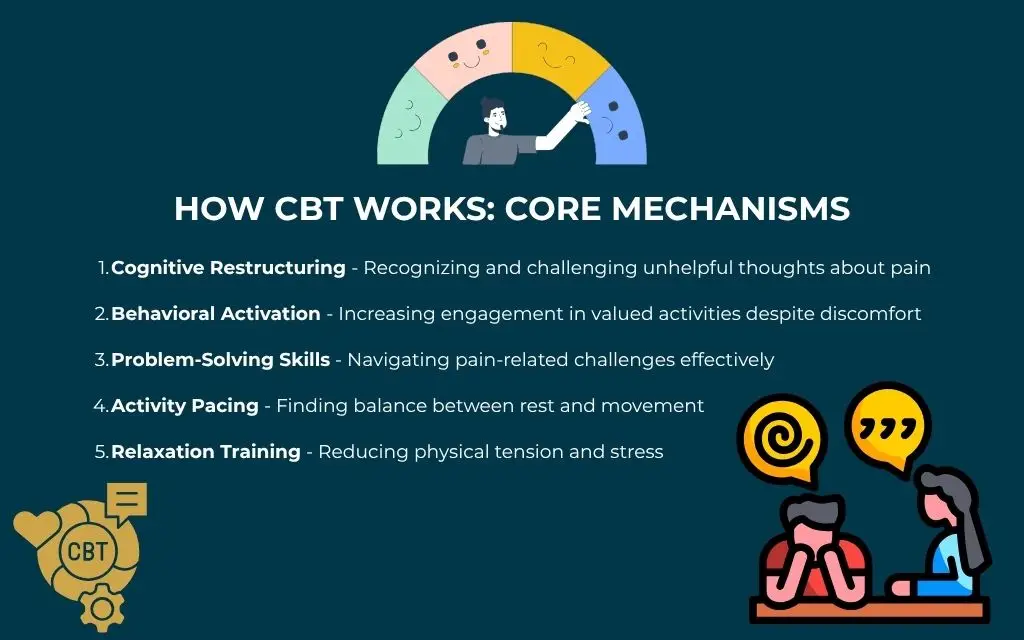
The American Psychological Association recognizes Cognitive Behavioral Therapy as the gold standard for chronic pain treatment. CBT for chronic pain helps you identify and change thought patterns and behaviors that worsen pain.
How CBT Works: Core Mechanisms
- Cognitive Restructuring – Recognizing and challenging unhelpful thoughts about pain
- Behavioral Activation – Increasing engagement in valued activities despite discomfort
- Problem-Solving Skills – Navigating pain-related challenges effectively
- Activity Pacing – Finding balance between rest and movement
- Relaxation Training – Reducing physical tension and stress
Research consistently shows CBT reduces pain intensity, improves physical function, and effectively treats co-occurring depression and anxiety. Studies demonstrate benefits lasting months and years after treatment ends.
During CBT sessions, you work collaboratively with your therapist. Together, you explore how thoughts influence emotions and behaviors. You learn practical skills for managing pain flares, pacing activities, and maintaining progress.
Denver residents seeking chronic pain therapy Denver can access qualified CBT providers trained specifically in pain psychology Colorado. Treatment typically involves 12 to 16 weekly sessions, with homework practice between appointments.
Acceptance and commitment therapy for chronic pain
Acceptance and Commitment Therapy takes a different approach than trying to eliminate pain. ACT helps you build psychological flexibility, allowing you to live fully even when pain persists.
The Six Core Processes of ACT:
- Acceptance – Embracing difficult experiences without struggling against them
- Cognitive Defusion – Creating distance from unhelpful thoughts
- Present Moment Awareness – Staying grounded in the here and now
- Self as Context – Recognizing you are more than your pain
- Values Clarification – Identifying what truly matters to you
- Committed Action – Taking steps aligned with your values
Research shows ACT improves pain acceptance, quality of life, and functional outcomes at six-month follow-up. The approach proves particularly effective when pain won’t fully resolve, helping you engage in meaningful activities regardless of discomfort.
ACT often incorporates mindfulness practices. You learn to observe pain without judgment, creating space between pain sensations and your response to them. This psychological flexibility allows movement toward values-based living.
Pain reprocessing therapy as breakthrough approach
Pain Reprocessing Therapy represents a newer treatment showing remarkable results. An NIH-funded clinical trial demonstrated that 66% of patients achieved pain-free or nearly pain-free status after just eight sessions. This success rate far exceeds the 20% improvement seen in placebo groups.
PRT specifically targets neuroplastic pain, teaching your brain to reinterpret pain signals as safe rather than dangerous. The treatment involves reattribution, helping you understand that pain doesn’t necessarily signal tissue damage, and exposure, gradually engaging in feared movements.
The “unlearning” process works through neuroplasticity. Your brain formed neural pathways that generate pain. Through PRT, you can develop new pathways that process sensations differently.
Best candidates for PRT include people with primary chronic back pain or widespread pain without clear structural causes. When medical imaging shows minimal damage yet pain persists, neuroplastic mechanisms likely contribute.
Mindfulness-based stress reduction and other approaches
Mindfulness-Based Stress Reduction offers an eight-week structured program combining mindfulness meditation and gentle yoga. MBSR teaches present-moment awareness, helping you respond to pain with less reactivity.
Biofeedback provides another evidence-based option. This technique teaches conscious control over physiological processes like muscle tension, heart rate, and breathing patterns. As you gain control, pain and stress often decrease.
Relaxation training includes progressive muscle relaxation, breathing exercises, and guided imagery. These techniques calm your nervous system, reducing the heightened arousal that amplifies pain.
Operant behavioral therapy focuses on reinforcing healthy behaviors while reducing pain behaviors. The approach recognizes that responses to pain can inadvertently maintain disability.
Interdisciplinary pain programs combine psychological treatment with medical care and rehabilitation. These comprehensive programs address all aspects of chronic pain through coordinated, collaborative care.
How mental health treatment actually reduces physical pain
Breaking the pain cycle
Chronic pain creates interconnected cycles involving physical sensations, thoughts, emotions, and behaviors. Each element influences the others, creating patterns that maintain suffering.
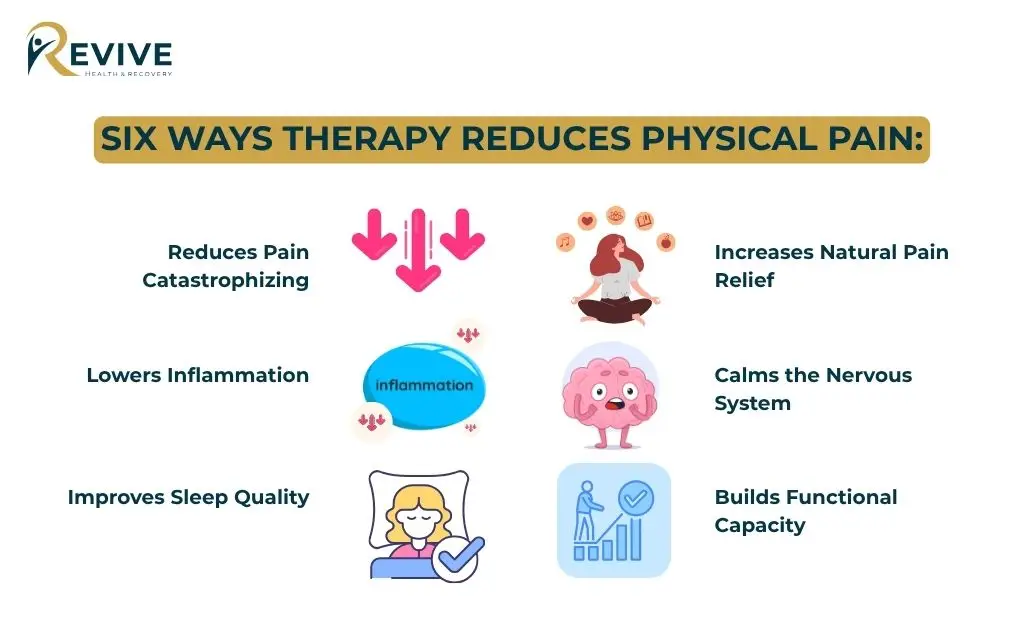
Six Ways Therapy Reduces Physical Pain:
- Reduces Pain Catastrophizing – Decreasing magnification and helplessness lowers nervous system reactivity and stress hormones
- Lowers Inflammation – Managing thoughts and emotions decreases inflammation markers in the body
- Improves Sleep Quality – Better sleep raises pain thresholds and reduces sensitivity
- Increases Natural Pain Relief – Behavioral activation releases endorphins and builds physical conditioning
- Calms the Nervous System – Relaxation techniques reduce heightened arousal that amplifies pain
- Builds Functional Capacity – Gradual activity increases strength and flexibility
Retraining your brain’s pain response
Your nervous system can develop pain memories. Neural pathways form that generate pain signals even without ongoing tissue damage. These learned patterns can be unlearned through neuroplasticity.
Exposure-based techniques reduce fear-avoidance gradually. You approach feared movements in controlled, safe ways. As your brain receives information that movement is safe, pain responses often decrease.
Pacing strategies help you find the balance between activity and rest. Rather than pushing through pain until you crash, pacing teaches sustainable engagement. You build tolerance gradually, avoiding flares that reinforce fear.
Activity modification doesn’t mean giving up valued pursuits. Instead, you learn adaptive approaches that allow participation. Small adjustments can mean the difference between avoidance and engagement.
Developing effective coping skills
Thought reframing helps you respond to pain with more helpful perspectives. Rather than thinking “This pain will never end,” you might recognize “Pain fluctuates, and I have tools to manage difficult moments.”
Cognitive defusion creates distance from thoughts without necessarily changing them. You observe thoughts as mental events rather than absolute truths.
Distraction and attention shifting provide practical relief during pain flares. Engaging fully in activities that matter to you naturally shifts attention away from pain.
Self-compassion practices reduce the additional suffering that comes from self-criticism. Many people with chronic pain blame themselves. Developing kindness toward yourself eases emotional distress.
Goal-setting and values-based living help you focus on what matters most. When pain limits some activities, clarifying values guides you toward meaningful alternatives.
Who benefits from mental health treatment for chronic pain
Ideal candidates for pain psychology services
Mental health treatment for chronic pain works best for people whose pain has persisted beyond three months despite medical interventions.
You may be a good candidate if you:
- Experience pain lasting three or more months despite medical treatment
- Face co-occurring depression, anxiety, or PTSD alongside pain
- Notice high levels of worry, fear, or negative thinking about pain
- Feel motivated to try approaches beyond medication
- Want to explore connections between mind and body
- Find that pain significantly limits work, relationships, or daily activities
- Feel open to learning new coping strategies
- Recognize that stress and emotions affect your pain levels
People ready to try non-medication approaches and willing to explore the mind-body connection tend to achieve the best results. Mental health treatment requires active participation and practice between sessions.
Functional impairment affecting work, relationships, or daily activities suggests that pain has created broader life challenges. Pain psychology helps you rebuild capabilities and reconnect with valued pursuits.
What to expect in your journey to pain relief in Denver
The first session with assessment and goal-setting
Your initial appointment focuses on understanding your unique pain story. Your therapist conducts a comprehensive assessment exploring pain history, triggers, impact on daily life, and previous treatments.
You’ll discuss how pain affects mood, sleep, relationships, work, and activities. This holistic picture helps identify treatment priorities.
Goal-setting happens collaboratively. Perhaps you want to reduce pain intensity, improve physical function, manage stress better, or address co-occurring depression. Your goals guide treatment planning.
Psychoeducation begins immediately. Your therapist explains connections between thoughts, emotions, and pain. Understanding these relationships empowers you to use treatment tools effectively.
Creating your personalized treatment plan involves selecting approaches that match your needs. Some people benefit most from CBT for chronic pain, while others respond better to ACT or mindfulness practices.
The environment remains supportive and judgment-free. You’re not expected to have everything figured out. Your therapist understands that chronic pain creates complex challenges requiring patience and compassion.
Treatment timeline and session structure
What to Expect During Treatment:
| Treatment Aspect | Details |
| Duration | 8 to 16 weekly sessions (varies by approach) |
| Session Length | 50 to 60 minutes per session |
| Homework | Practice activities between sessions |
| Progress Tracking | Regular monitoring to identify patterns and improvements |
| Adjustments | Flexible modifications based on your response |
| PRT Timeline | Often shows results within 8 sessions |
Skills learned in therapy become effective through regular use. Your therapist assigns manageable practice activities tailored to your life.
Progress tracking helps you see improvements that might otherwise go unnoticed. Pain fluctuates naturally, making systematic tracking valuable for recognizing patterns and gains.
Maintenance and long-term management strategies prepare you for life after formal treatment ends. You’ll develop plans for sustaining gains and addressing future challenges.
Combining mental health treatment with medical care
The most effective approach combines mental health treatment for chronic pain with appropriate medical care. This integrated biopsychosocial model addresses all contributing factors.
You’ll continue working with your medical providers while receiving therapy. Your pain management doctor, primary care physician, and other specialists remain part of your care team.
At Revive Health Recovery, we coordinate with your healthcare providers when appropriate. Communication between professionals ensures everyone understands your treatment plan.
Our outpatient healing center offers flexible treatment that fits your life. You’re not admitted to a hospital. Instead, you attend scheduled appointments while maintaining your normal routine.
This coordinated, comprehensive care maximizes outcomes. Physical treatments address tissue-level factors. Psychological treatments address brain and nervous system contributions. Together, they create powerful synergy.
Insurance, costs, and accessibility in Colorado
Does insurance cover mental health treatment for chronic pain?
The federal Mental Health Parity and Addiction Equity Act requires insurance companies to cover mental health services equally with medical services. This law protects access to pain psychology treatment.
Most insurance plans cover therapy for chronic pain under behavioral health benefits. Coverage applies when treating co-occurring depression, anxiety, or when using psychological approaches for pain management.
Typical Insurance Coverage:
| Coverage Type | What to Expect |
| Copays | Usually $20 to $50 per session |
| After Deductible | Some plans cover 100% of session costs |
| Medicare | Covers pain psychology services with qualified providers |
| Medicaid | Covers mental health treatment for chronic pain |
| Coverage Varies | Specific benefits depend on your individual plan |
Verifying your specific benefits takes just a phone call. Contact Revive Health Recovery at (303) 268-4655, and our staff will check your coverage details. We accept most major insurance plans.
Making treatment affordable and accessible
Revive Health Recovery works with insurance companies to make mental health treatment for chronic pain accessible. We handle the billing complexities, allowing you to focus on healing.
For people without insurance or with limited coverage, we offer options to make treatment affordable. Discussing your situation with our intake staff helps identify solutions.
Health Savings Accounts and Flexible Spending Accounts cover mental health treatment as qualified medical expenses. Using these pre-tax dollars reduces your out-of-pocket costs.
Consider the long-term value. Ongoing medical appointments, medications, and procedures create sustained expenses. Effective mental health treatment can reduce these costs by addressing pain more comprehensively.
Our Denver location at 1427 S Federal Blvd offers convenient access. Public transportation serves the area well. Ample parking accommodates those driving.
Telehealth options for Colorado residents
Virtual therapy sessions provide convenient alternatives to in-person appointments. Telehealth mental health treatment for chronic pain proves equally effective for many approaches.
People with mobility limitations particularly benefit from telehealth. Traveling to appointments can worsen pain. Virtual sessions eliminate this barrier.
Rural Colorado residents gain access to specialized pain psychology Colorado services through telehealth. Geographic distance no longer limits treatment options.
All telehealth platforms meet HIPAA compliance standards, protecting your privacy and confidentiality. Secure connections ensure your health information remains protected.
Why choose Revive Health Recovery for chronic pain treatment
Our evidence-based approach to pain psychology
Revive Health Recovery specializes in mental health treatment for chronic pain using approaches backed by rigorous research. Our therapists receive specialized training in pain psychology, understanding the unique challenges chronic pain creates.
Comprehensive biopsychosocial assessment identifies all factors contributing to your pain experience. We look beyond symptoms to understand your complete story.
Personalized treatment plans combine proven approaches including CBT for chronic pain, Acceptance and Commitment Therapy, mindfulness practices, and other evidence-based techniques. Your treatment matches your specific needs.
Trauma-informed care recognizes that adverse experiences can contribute to chronic pain. When pain involves PTSD or past trauma, we address these connections sensitively and effectively.
Our healing environment differs from clinical hospital settings. We’ve created welcoming, comfortable spaces that promote relaxation and openness.
Outpatient treatment that fits your life
Revive Health Recovery operates as an outpatient healing center, not an inpatient hospital. This distinction matters for your daily life.
Flexible scheduling includes evening and weekend appointments. You don’t need extended time off work. Treatment fits around your responsibilities.
You continue living at home, maintaining family connections and normal routines. This continuity supports long-term success.
Our comfortable Denver location provides easy access without the institutional feel of hospital-based programs.
We’re available 24/7 at (303) 268-4655 for questions or concerns. Accessible support helps you feel confident throughout treatment.
Comprehensive support beyond individual therapy
Treatment at Revive Health Recovery extends beyond individual therapy sessions. We coordinate with your medical providers to ensure integrated care.
Group therapy options connect you with others facing similar challenges. Shared experiences reduce isolation and provide mutual support.
Family education and support recognize that chronic pain affects entire families. When loved ones understand your experience, they can support your recovery more effectively.
Relapse prevention and maintenance planning prepare you for sustaining gains. You’ll develop strategies for managing future challenges independently.
Denver community resources and connections help you build broader support networks. Recovery flourishes when you feel connected to your community.
Taking the first step toward pain relief
How to get started with mental health treatment
Starting mental health treatment for chronic pain requires just one phone call. Contact Revive Health Recovery at (303) 268-4655. We’re available 24/7 to answer questions and schedule appointments.
Your Simple Path to Getting Started:
Step 1: Call (303) 268-4655 or email contact@revivehealthrecovery.com
Step 2: Speak with our compassionate intake staff about your needs
Step 3: We verify your insurance coverage and answer cost questions
Step 4: Schedule your first appointment at a convenient time
Step 5: Receive confirmation and preparation information
Visit our Denver location at 1427 S Federal Blvd, Denver, CO 80219. Our welcoming space reflects our commitment to comfortable, supportive care.
You’ll encounter no judgment, only understanding and hope. Everyone at Revive Health Recovery recognizes the courage required to seek help.
Preparing for your first appointment
Bringing a list of current medications and relevant medical records can help, though neither is required. Your therapist uses this information to understand your complete picture.
Prepare to discuss your pain history and how pain affects your life. Honest, open communication helps your therapist develop the most effective treatment plan.
Write down questions or concerns before your appointment. This preparation ensures you address everything important to you.
Wear comfortable clothing. Physical comfort supports mental ease during your session.
Arrive with an open mind and willingness to explore new approaches. Curiosity about how mental health treatment for chronic pain works helps you engage fully.
Remember that seeking help demonstrates strength. You’re taking a brave step toward healing.
FAQs about mental health treatment for chronic pain
Is my chronic pain all in my head?
Your chronic pain is absolutely real, not imagined. Pain always involves brain processing, meaning psychological factors influence intensity. Mental health treatment doesn’t dismiss your pain. Instead, it provides additional tools by addressing how your brain processes pain signals. Research shows psychological therapies reduce pain as effectively as many medical treatments because pain involves mind-body interactions. At Revive Health Recovery in Denver, we validate your pain while offering evidence-based approaches that work.
How does therapy actually reduce physical pain symptoms?
Therapy reduces pain through multiple mechanisms. First, it decreases pain catastrophizing and fear that amplify pain signals. Second, it lowers stress hormones and inflammation. Third, relaxation techniques calm your nervous system. Fourth, improved sleep decreases pain sensitivity. Fifth, increased activity releases natural endorphins. Sixth, brain retraining helps you interpret pain signals as less threatening. Brain imaging confirms these therapies change pain processing. Revive Health Recovery specializes in these evidence-based approaches.
How long does mental health treatment for chronic pain take to work?
Most patients notice improvements within four to eight weeks. Cognitive Behavioral Therapy typically involves 12 to 16 sessions. Pain Reprocessing Therapy shows results in as few as eight sessions, with 66% of patients achieving significant relief. Mindfulness programs run eight weeks. Benefits often continue growing after treatment ends as you apply learned skills. Your Revive Health Recovery therapist tracks progress and adjusts approaches based on your response.
Will I have to stop taking pain medications or seeing my doctor?
No. Mental health treatment for chronic pain works best alongside comprehensive medical care. You’ll continue seeing your medical providers and maintain appropriate medications. The goal adds psychological tools to your pain management approach. Revive Health Recovery coordinates with your healthcare team for seamless, collaborative treatment. Many patients eventually reduce medication use as psychological skills improve pain management, though this happens gradually and with medical guidance.
Does insurance really cover therapy for chronic pain?
Yes. The federal Mental Health Parity and Addiction Equity Act requires equal coverage for mental health services. Therapy for chronic pain-related depression, anxiety, or pain management typically falls under behavioral health benefits. Most plans cover treatment with copays of $20 to $50 per session. Some cover 100% after deductibles. Medicare and Medicaid cover pain psychology services. Revive Health Recovery accepts most insurance plans. Call (303) 268-4655 for coverage verification.
Your path to relief starts with understanding
Mental health treatment for chronic pain recognizes that suffering involves intricate connections between body, brain, and emotions. Evidence-based approaches including Cognitive Behavioral Therapy, Acceptance and Commitment Therapy, and Pain Reprocessing Therapy have helped thousands reduce chronic pain by addressing psychological factors. Whether you experience fibromyalgia, chronic back pain, or persistent pain unresponsive to medical treatments alone, psychological therapy offers powerful healing tools. The relationship between mental health and chronic pain works bidirectionally, meaning treating one improves the other.
At Revive Health Recovery in Denver, we specialize in evidence-based mental health treatment for chronic pain, helping Colorado residents break free from pain cycles. Our comprehensive approach combines proven techniques with compassionate care in a supportive outpatient setting.
You don’t have to continue suffering or feeling dismissed by providers focusing only on physical treatments. Recovery becomes possible when you address both physical and psychological aspects of chronic pain.
Take the first step toward relief today. At Revive Health Recovery, our team understands chronic pain’s toll on every aspect of life. We provide specialized, evidence-based mental health treatment in Denver that empowers you to reclaim quality of life.
Call us anytime at (303) 268-4655
Email contact@revivehealthrecovery.com
Visit us at 1427 S Federal Blvd, Denver, CO 80219
Revive Health Recovery is an outpatient healing center offering flexible treatment that fits your life. Insurance accepted. Free consultations available. Your journey to pain relief starts with one phone call.



