Explore a complete though about what is involuntary mental health treatment here. When a loved one experiences a severe mental health crisis, families often face difficult decisions about treatment options. In Colorado, involuntary mental health treatment serves as a last resort when someone poses an imminent danger to themselves or others but refuses voluntary care.
This comprehensive guide explains Colorado’s specific laws, processes, and patient rights surrounding involuntary commitment. We help Denver-area families understand their options during these challenging times. From the initial 72-hour M-1 hold to long-term treatment considerations, we explore every aspect of this complex system while highlighting alternatives that prioritize recovery and dignity.
Understanding Colorado’s involuntary mental health treatment system
Legal foundation under Colorado Revised Statute 27-65
Colorado’s involuntary mental health treatment operates under strict legal guidelines established by Colorado Revised Statute 27-65. This comprehensive legislation governs how mental health professionals, courts, and treatment facilities handle emergency psychiatric situations.
The Colorado Behavioral Health Administration (BHA) oversees the implementation of these laws across the state. They ensure designated treatment facilities meet specific requirements for handling involuntary patients. These facilities must maintain proper staffing, documentation protocols, and patient rights protections.
The statute establishes clear criteria for when involuntary treatment becomes necessary. It protects both patient rights and public safety while providing a framework for crisis intervention. Denver-area families benefit from these structured protections during mental health emergencies.
The M-hold classification system
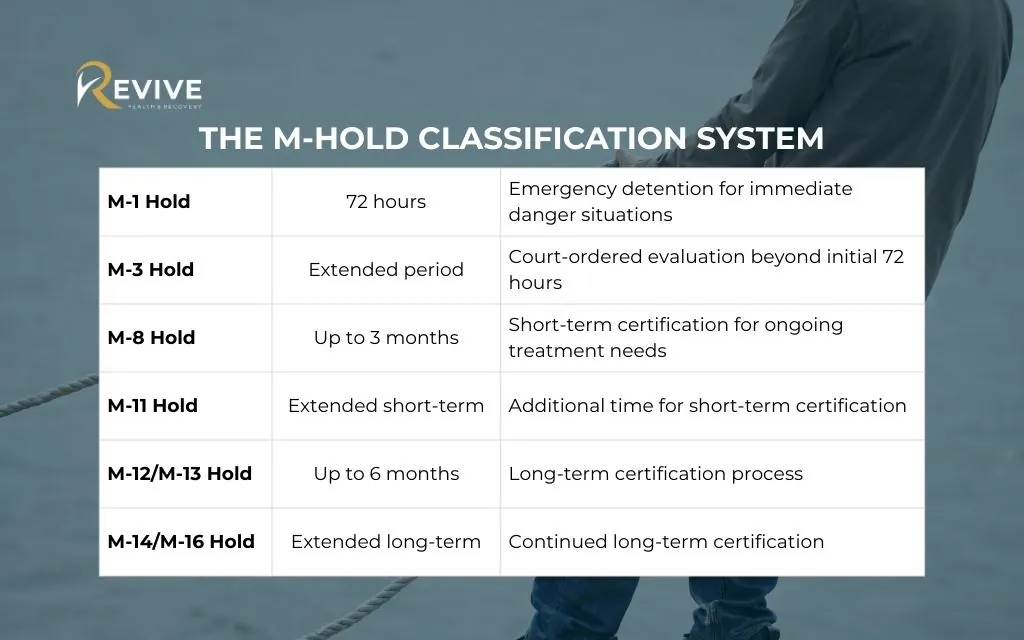
Colorado uses a unique M-hold system that differs from other states’ approaches. This system provides specific designation codes for different stages of involuntary mental health treatment.
| Hold Type | Duration | Purpose |
| M-1 Hold | 72 hours | Emergency detention for immediate danger situations |
| M-3 Hold | Extended period | Court-ordered evaluation beyond initial 72 hours |
| M-8 Hold | Up to 3 months | Short-term certification for ongoing treatment needs |
| M-11 Hold | Extended short-term | Additional time for short-term certification |
| M-12/M-13 Hold | Up to 6 months | Long-term certification process |
| M-14/M-16 Hold | Extended long-term | Continued long-term certification |
This structured approach ensures appropriate levels of intervention based on individual circumstances and treatment progress.
Criteria for involuntary mental health treatment in Colorado
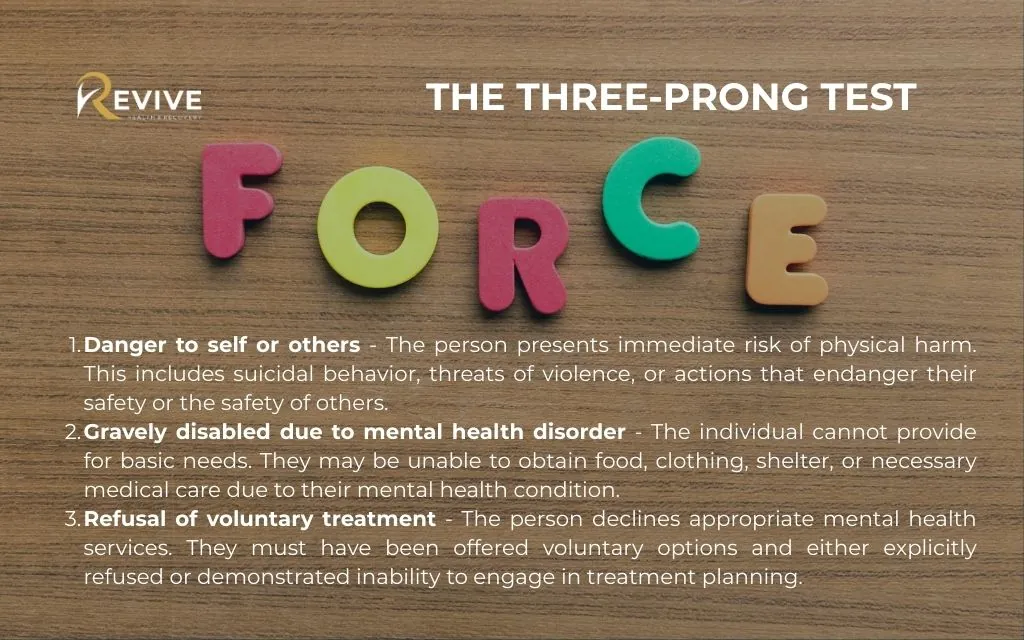
The three-prong test
Colorado law requires meeting specific criteria before implementing involuntary mental health treatment. Mental health professionals must demonstrate all three elements exist simultaneously:
- Danger to self or others – The person presents immediate risk of physical harm. This includes suicidal behavior, threats of violence, or actions that endanger their safety or the safety of others.
- Gravely disabled due to mental health disorder – The individual cannot provide for basic needs. They may be unable to obtain food, clothing, shelter, or necessary medical care due to their mental health condition.
- Refusal of voluntary treatment – The person declines appropriate mental health services. They must have been offered voluntary options and either explicitly refused or demonstrated inability to engage in treatment planning.
Who can initiate an involuntary hold
Several qualified professionals can begin the involuntary mental health treatment process in Colorado:
- Licensed mental health professionals – Frequently initiate holds when working with clients in crisis
- Medical doctors and registered nurses – Can start the process under specific conditions with proper documentation
- Law enforcement officers – May initiate holds during crisis calls or emergency situations
- Court system – Becomes involved when extended treatment beyond initial emergency holds appears necessary
Each professional must document their observations and provide clear evidence supporting the three-prong test criteria.
The step-by-step process of involuntary commitment
Emergency response and initial hold
When someone experiences a mental health crisis requiring immediate intervention, crisis teams respond quickly. Colorado Crisis Services (988) provides 24/7 support and can dispatch mobile crisis teams to assess situations.
Transportation to designated facilities occurs once professionals determine involuntary hold criteria are met. Specialized vehicles and trained personnel ensure safe transport while maintaining the person’s dignity.
Initial screening happens immediately upon arrival at the treatment facility. Mental health professionals conduct comprehensive assessments to confirm the need for continued involuntary treatment.
72-hour evaluation period
The evaluation period begins once the M-1 hold takes effect. Mental health professionals assess the individual’s condition, review their history, and develop initial treatment recommendations.
Colorado law requires continuous evaluation for voluntary status throughout this period. If the person no longer meets involuntary criteria, they must be released or offered voluntary treatment options.
Patient rights remain protected during evaluation. Individuals receive information about their legal protections, access to communication, and the right to request legal representation.
Court proceedings and legal protections
When treatment needs extend beyond 72 hours, petition filing with the court becomes necessary. Mental health professionals provide detailed documentation supporting continued involuntary treatment.
Legal representation rights ensure every person has access to qualified counsel. Public defenders specializing in mental health law represent individuals who cannot afford private attorneys.
Hearing procedures follow strict guidelines protecting constitutional rights. Judges review evidence, hear testimony, and make decisions based on clear legal standards rather than convenience or availability of services.
Patient rights during involuntary treatment
Constitutional protections
Due process requirements protect individuals throughout the involuntary mental health treatment process. Courts must follow established procedures and provide fair hearings before extending involuntary commitment.
The right to legal counsel ensures proper representation during proceedings. Attorneys advocate for their clients’ interests and challenge evidence when appropriate.
Appeal rights and habeas corpus protections allow individuals to contest their involuntary status. They can request judicial review of their detention and treatment orders.
Treatment rights and dignity
The least restrictive environment principle guides treatment decisions. Facilities must provide care in settings that maximize independence while ensuring safety and therapeutic benefit.
Privacy and confidentiality protections continue during involuntary treatment. Personal information, treatment records, and communications remain protected under state and federal law.
Family involvement considerations balance patient autonomy with support system benefits. Treatment teams work to include family members when appropriate and with patient consent.
Voting rights and civil liberties remain intact during treatment. Involuntary commitment does not automatically remove other legal rights or civil protections.
Denver-specific resources and services
Crisis intervention programs
- Colorado Crisis Services (988) Available 24/7 through phone, text, or chat Crisis counselors provide immediate support Can coordinate emergency response when needed
- The STAR Program Denver’s innovative crisis response approach Pairs mental health professionals with paramedics Responds instead of police officers for mental health emergencies
- Denver Health Psychiatric Emergency Services Specialized emergency departments for mental health crises Immediate assessment and stabilization services Expert staff trained in crisis intervention
- WellPower Crisis Services Community-based crisis intervention throughout Denver metro Mobile teams respond to homes, schools, and community locations Comprehensive support during crisis situations
Designated treatment facilities in Denver area
Hospital-based psychiatric units provide intensive inpatient care for individuals requiring medical stabilization. These facilities handle complex cases requiring 24-hour monitoring.
Community mental health centers offer specialized programs for involuntary patients transitioning to outpatient care. They provide ongoing support and treatment coordination.
Specialized treatment programs address specific populations such as adolescents, older adults, or individuals with co-occurring disorders. These programs tailor approaches to unique needs.
Alternatives to involuntary commitment
Voluntary treatment options
- Outpatient therapy and counseling provide effective treatment while allowing individuals to remain in their communities. Licensed therapists offer individual, group, and family sessions.
- Intensive outpatient programs (IOP) deliver structured treatment several hours per day while permitting people to return home each evening. These programs bridge the gap between inpatient and traditional outpatient care.
- Partial hospitalization programs offer day treatment with comprehensive services. Participants receive therapy, medication management, and skills training during daytime hours.
- Peer support services connect individuals with others who have experienced similar challenges. Peer specialists provide guidance, encouragement, and practical assistance.
Crisis prevention strategies
Early intervention programs identify warning signs before crises develop. Mental health professionals work with individuals and families to recognize symptoms and implement coping strategies.
Family education and support help loved ones understand mental health conditions and effective response strategies. Education reduces fear and improves family dynamics during difficult periods.
Crisis planning involves developing written plans outlining specific steps to take when symptoms worsen. These plans include contact information, preferred treatments, and advance directives.
Community-based resources provide ongoing support through support groups, recreational programs, and social services. These connections reduce isolation and promote wellness.
The role of families in the process
Supporting a loved one through crisis
Understanding warning signs helps families recognize when professional intervention becomes necessary. Common signs include dramatic behavior changes, threats of self-harm, or inability to care for basic needs.
Navigating the legal process can feel overwhelming for families. Understanding rights, procedures, and timelines helps families advocate effectively for their loved ones.
Advocacy and communication strategies enable families to work collaboratively with treatment teams. Clear communication improves treatment outcomes and reduces stress.
Long-term recovery planning involves families in developing sustainable support systems. Recovery extends beyond crisis resolution to include ongoing wellness maintenance.
When to consider involuntary treatment
Safety assessment considerations guide difficult decisions about involuntary intervention. Families must weigh immediate safety concerns against autonomy and relationship preservation.
Exhausting voluntary options demonstrates good faith efforts to avoid involuntary measures. Documentation of refused services strengthens cases when involuntary treatment becomes necessary.
Working with mental health professionals provides expert guidance during decision-making. Professionals can assess situations objectively and recommend appropriate interventions.
Legal consultation offers families understanding of their options and potential outcomes. Attorneys specializing in mental health law provide valuable guidance.
Recovery and transition planning
From involuntary to voluntary care
Building therapeutic relationships becomes crucial for successful transition to voluntary treatment. Trust develops gradually as individuals experience respectful, effective care.
Addressing underlying issues requires comprehensive assessment and treatment planning. Root causes of mental health challenges need attention beyond crisis stabilization.
Medication management and compliance support help individuals understand treatment benefits. Education about medications reduces fears and improves adherence.
Developing coping strategies provides tools for managing future challenges. Skills training helps individuals handle stress, relationships, and daily responsibilities.
Long-term support systems
Colorado’s peer navigation services offer unique support for individuals who have experienced involuntary commitment. These programs provide $2.5 million in funding specifically for peer support.
Community integration programs help individuals rebuild connections and independence. Services include housing assistance, employment support, and social skills training.
Ongoing mental health maintenance prevents future crises through regular monitoring and support. Consistent care reduces the likelihood of repeated involuntary interventions.
Family therapy and education strengthen support systems for long-term success. Healthy family dynamics contribute significantly to sustained recovery.
Recent changes in Colorado mental health law
2023 legislative reforms
Enhanced patient rights protections strengthen safeguards during involuntary treatment. New requirements ensure better communication, representation, and appeal processes.
Improved data collection requirements help Colorado track outcomes and identify system improvements. This information guides policy decisions and resource allocation.
Expanded treatment options provide alternatives to traditional hospital-based care. Community programs receive support for innovative approaches to crisis intervention.
The impact on Denver-area services includes increased funding for community programs and enhanced training for crisis response teams. These improvements benefit families throughout the region.
FAQs about what is involuntary mental health treatment
How long can someone be held involuntarily for mental health treatment in Colorado?
Initial M-1 holds last 72 hours, with possible extensions through court proceedings. Short-term certifications can extend up to three months, while long-term certifications may last six months or longer. Each extension requires court review and must meet specific legal criteria. Contact Revive Health Recovery to discuss alternatives that may prevent the need for extended involuntary treatment.
What are the costs associated with involuntary mental health treatment?
Costs vary depending on the facility, length of stay, and services provided. Insurance coverage, including Medicaid and private insurance, typically covers medically necessary involuntary treatment. For specific cost information and insurance verification, contact Revive Health Recovery at (303) 268-4655. Our team can help you understand coverage options and affordable alternatives.
Can family members request an involuntary hold for their loved one?
Family members cannot directly initiate involuntary holds, but they can contact qualified professionals who can assess the situation. Call Colorado Crisis Services at 988 or contact local emergency services if immediate intervention appears necessary. Revive Health Recovery can help families understand the process and explore voluntary treatment options before crisis situations develop.
What happens if someone refuses medication during involuntary treatment?
Colorado law protects the right to refuse medication except in emergency situations. Courts may order medication in specific circumstances after careful review and legal proceedings. Treatment teams work to educate patients about medication benefits and address concerns. Revive Health Recovery emphasizes collaborative medication management that respects patient preferences while ensuring safety.
Are there alternatives to hospitalization for someone in a mental health crisis?
Yes, Colorado offers numerous alternatives including intensive outpatient programs, crisis stabilization services, mobile crisis teams, and community-based support. Early intervention often prevents the need for involuntary hospitalization. Revive Health Recovery specializes in comprehensive outpatient services that provide effective crisis intervention while maintaining independence and dignity.
Find compassionate mental health support at Revive Health Recovery
At Revive Health Recovery in Denver, we understand that mental health crises affect entire families. While we don’t provide inpatient services, our comprehensive outpatient programs offer effective alternatives to hospitalization. Our experienced team specializes in crisis intervention, intensive outpatient therapy, and family support services designed to help individuals achieve lasting recovery while maintaining their dignity and independence.
Located at 1427 S Federal Blvd, Denver, CO 80219, we provide personalized treatment plans that address the root causes of mental health challenges. Our evidence-based approaches include individual therapy, group counseling, family therapy, and psychiatric care. All services focus on preventing future crises and promoting long-term wellness.
Our team works collaboratively with families to develop comprehensive safety plans and coping strategies. We understand Colorado’s involuntary mental health treatment laws and can help you navigate these complex systems while exploring every possible alternative to involuntary commitment.
Conclusion
Understanding involuntary mental health treatment in Colorado empowers families to make informed decisions during crisis situations. While these legal protections serve an important purpose, the goal remains transitioning individuals to voluntary care that supports their recovery journey.
Early intervention and comprehensive outpatient services often prevent the need for involuntary treatment. Working with experienced mental health professionals provides families with tools and strategies for supporting loved ones through difficult periods.
If you or a loved one is struggling with mental health challenges, don’t wait for a crisis to occur. Contact Revive Health Recovery today to explore proactive treatment options that can prevent the need for involuntary intervention.
Ready to take the first step toward recovery?
Call us 24/7: (303) 268-4655
Email: contact@revivehealthrecovery.com
Visit us: 1427 S Federal Blvd, Denver, CO 80219
Our compassionate team is here to help you navigate these challenging times and find the path to lasting mental wellness. Together, we can develop strategies that protect your loved one’s safety while preserving their autonomy and dignity.



